Parkinson's Disease
and other Neurodegenerative Disorders
TREATMENT AND LIFESTYLE OPTIONS -- An Introduction
An Introduction to PD here
More in-depth information here
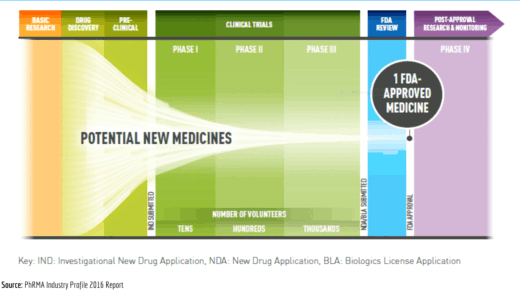
Parkinson's Disease can't be cured and living well in the presence of the disease can be a real struggle, frequently bringing to mind the concept of "fighting" the disease, with programs being named consistent with this, like "Rock Steady Boxing". However, a variety of medications and activities can help with controlling and dealing with the symptoms, sometimes dramatically. The graphics on the left convey that while many reseerch trials are being conducted on finding new drugs for the disease few "make the cut". Increasingly. however, drugs once used for other conditions, particularly some used for depression and diabetes are being "re-purposed" for use with Parkinson's (see Durães et al, 2018, for a discussion). As loss of dopamine is one of the primary underlying contributors to the symptoms of PD it's important that medication is taken to supplement the body's supply, often with a levodopa-based medication, and that such medication is taken appropriately -- as discussed in the second video below. The second video shows the introduction to the free training program for those interested in the principles of exercise for people with Parkinson's. This excellent program comes from the Brian Grant Foundation whose website also covers material on nutrition and on dealing better with activities of daily living. While exercise is regarded as being an essential complement to medication, it's important to make sure such exercise is conducted safely, as depicted below in the third video. The fourth video talks about one of the "oldest" neurostimulatory treatments used to help people for whom other forms of treatment, usually drugs, have lost their previous effectiveness. Newer methods are also now available, some of which have been found to improve higher cognitive functioning -- see the /TREATMENTS















SHARE THIS PAGE!