
Parkinson's Disease
and other Neurodegenerative Disorders
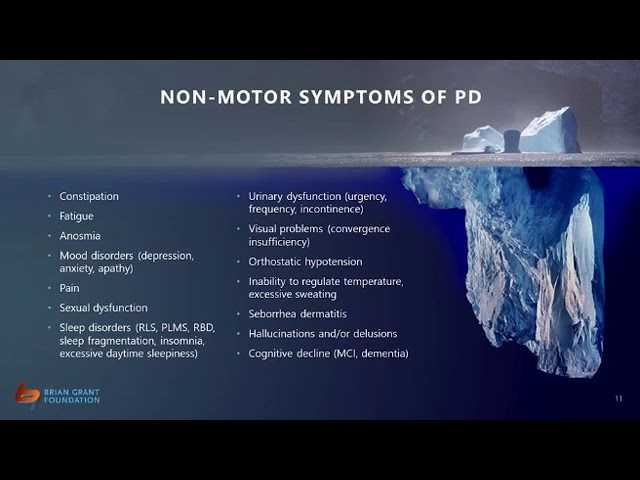
Parkinson's Disease is the second most common degenerative neurological disorder, after Alzheimer's. Age-at-diagnosis is typically in the early 60s, and it is slightly more common in men than in women. It can come to affect nearly every organ system in the body and is still regarded as incurable, though there are treatments that can help sufferers cope better with its symptoms. It is the focus of broad-ranging and extensive research.
Most importantly, it is NOT a fatal illness in itself.
Information on this site is drawn from a number of quality-checked or professional association sites. Links to external resources are highlighted and in a different color to the background.
Resources available on my Google drive are located in the folder the link is provided to, for example, /ETIOLOGY.
Read only access to my drive is available here
Access to my selected references via Mendeley are here
Further information on the sources for information provided are given in the next section "Information Sources"
This site discusses the nature of the disease, its symptoms and early signs, believed causes, treatments including complementary non-medical approaches, and guides to living well while having the disease. I was diagnosed as suffering from the disease in 2016, when aged 61. Hence, the focus in this section will be on what I know best, but some information on other neurodegenerative diseases is included along the way, given the simiilaritiess in etiology of these diseases (see, for example, Uddin and Amran, 2019). Indeed, when someone first sees a doctor, they will be likely to be said to be suffering from one or more "Parkinsonisms" -- see here, the final diagnosis not being given pending further investigation. A good general overview of Parkinson's Disease is provided in the first video below. As loss of dopamine is one of the primary underlying contributors to the symptoms of PD it's important that medication is taken to supplement the body's supply (see the second video below), Exercise is often regarded as being an essential complement to medication, and it's important to make sure such exercise is conducted safely, as depicted below in the third video. Indeed, it will be seen that while Parkinson's Disease is likely the product of a broad range of factors interacting with each other, it is the combined effects of exercise and dietary factors that provide the best means of avoiding, or at least delaying and dealing with the disease that provides the most hope and improved quality of life.






SHARE THIS PAGE!